Many people visit a physical therapist after seeing a physician and being given a prescription to start physical therapy. However,…

Another new year is upon us and with it comes the resolution to get in shape, lose weight, or commit…

Patellofemoral pain syndrome refers to pain in the front of the knee or around the kneecap (patella). It is the…

Knee arthritis is a condition where the protective cartilage of your joints breaks down. The cartilage serves as a pad…

Loss of range of motion in your hip may be causing you lower back pain. People with low back pain…

Have you tried all types of low back exercises for your lingering back pain? You might want to have your…

The leading cause of morbidity and mortality in the United States is chronic disease. Heart disease, stroke, cancer, diabetes and…

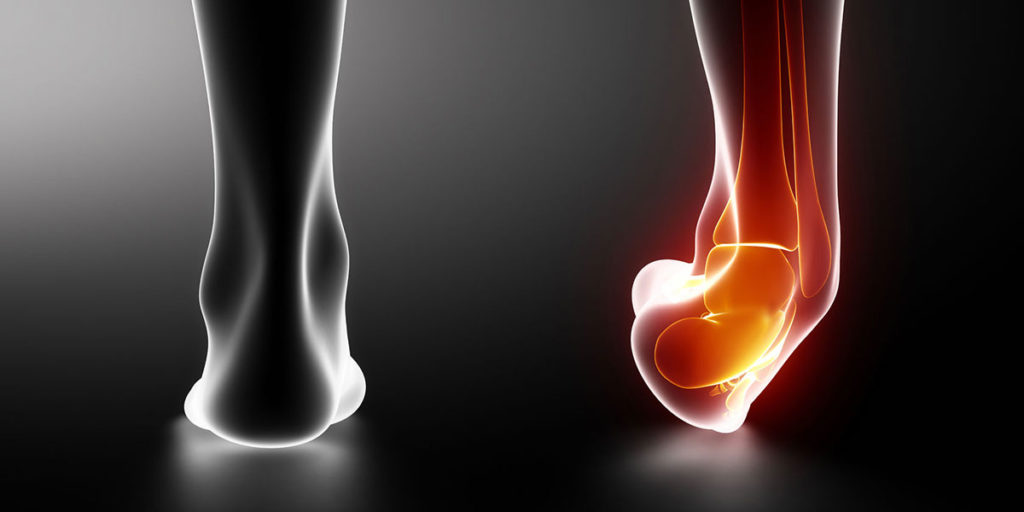
Plantar fasciitis is one of the most commonly treated types of foot pain in physical therapy. Overuse or repetitive stress…

What are Ankle Sprains? Ankle sprains are one of the most common injuries that people experience. These injuries account for…
Too many medical approaches in today’s society are dependent on others (therapists, doctors, etc) and include passive treatments (medications, injections,…
