Have you ever jumped out of bed with an intense cramp in your leg or foot? Nighttime leg cramps occur…

Hip pain occurs in 1 of every 4 women over the age of 50. Many men also experience annoying hip…

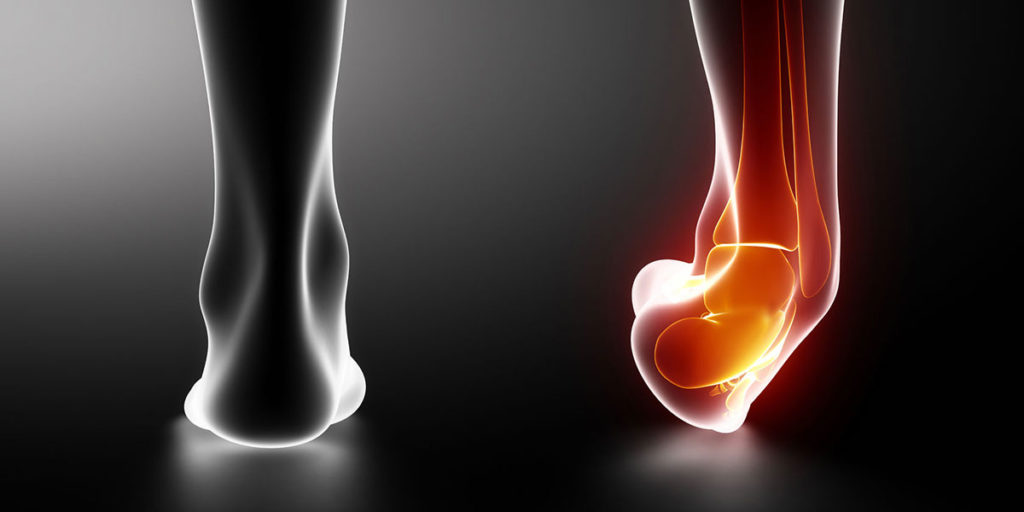
Painful Achilles tendon problems are common in people who perform repetitive running and jumping activities. It is also common in…

An estimated 1 of every 4 rotator cuff repairs will re-tear within 6 months of surgery. Overly aggressive rehabilitation or…

The leading cause of morbidity and mortality in the United States is chronic disease. Heart disease, stroke, cancer, diabetes, and…

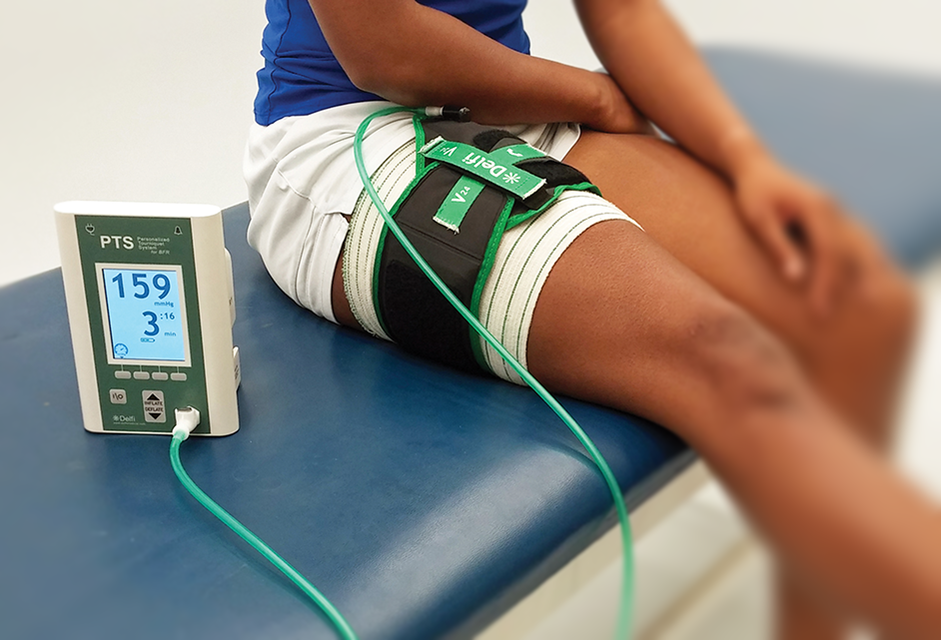
Blood flow restriction (BFR) therapy uses external pressure over a body part during exercise. The applied pressure allows the flow…
What are Ankle Sprains? Ankle sprains are one of the most common injuries that people experience. These injuries account for…
Low back injuries do not always occur from one single incident or event like lifting a heavy box. Instead, most…

The gluteus maximus is the most powerful hip extensor. This is important for functional activities performed in one plane such…
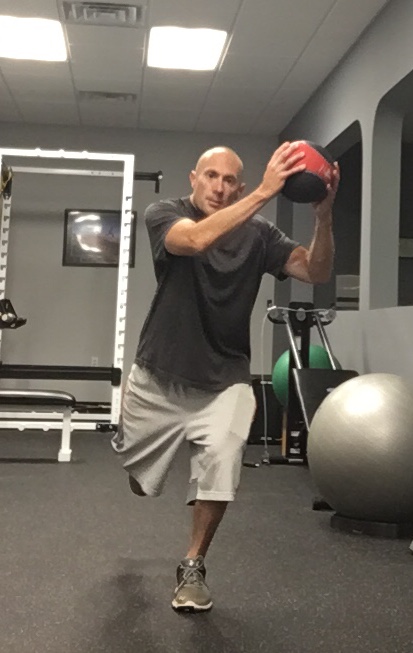
Typically training for power is thought of as something for young athletes. However, today older adults are staying more active…
