An estimated 250,000 anterior cruciate ligament (ACL) reconstruction surgeries are done each year. Unfortunately, surgery does not guarantee a return…

An estimated 850,000 meniscus surgeries are done each year in the U.S. Previously, we reviewed the keys to recovery after…

Meniscus surgery is the most common orthopedic procedure performed in the U.S. According to Harvard Medicine, 750,000 meniscus surgeries are…

Pain or tightness around your knee can be from poor hamstring flexibility. Research proves tight hamstrings contribute to knee pain. …

It can be frustrating when knee pain or an old injury interferes with your workouts. This is especially true when…

It is estimated that the number of knee replacement surgeries in the United States will increase by 673% from 2005…

The success of your knee replacement surgery depends on how you progress during your rehabilitation. In particular, the first few…
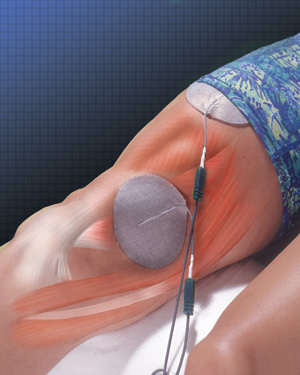
Knee replacement surgeries are helping hundreds of thousands of people each year. Most studies show 1-year patient satisfaction rates at…

If you are one of the millions of Americans bothered by hip or knee arthritis, this article is for you. …

Over 5 million people live in the U.S. with a total knee replacement. This number is rapidly growing. Knee replacement…
