Many people falsely believe ankle sprains get better on their own. Resting a sprained ankle and not getting the appropriate…

Shin splints are a common overuse injury in active teenagers, runners, and military personnel. It is characterized by diffuse pain…

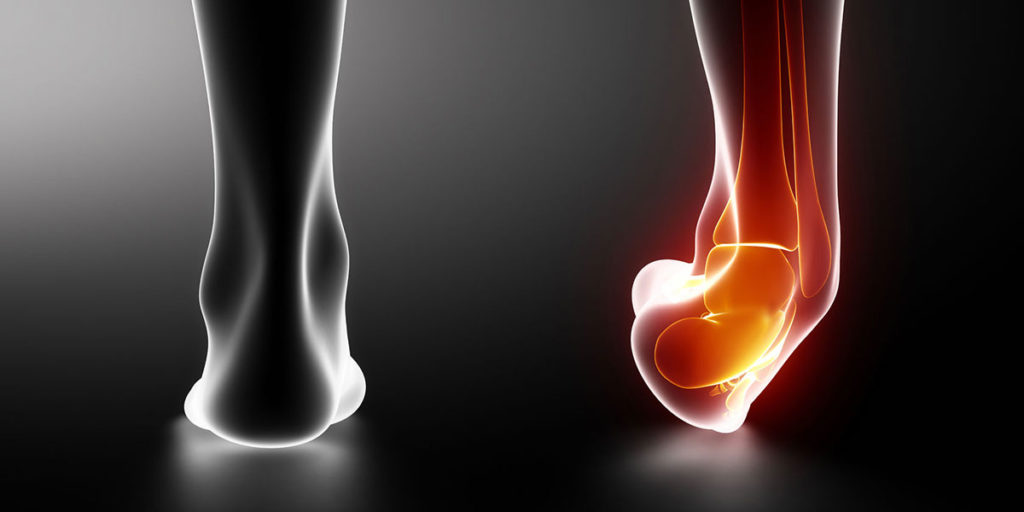
Many people are frustrated by persistent pain long after suffering an ankle sprain. Almost 3 out of every 4 people…

Are you struggling with Achilles tendon pain that won’t go away? Achilles tendinitis is one of the most stubborn injuries…

Have you ever jumped out of bed with an intense cramp in your leg or foot? Nighttime leg cramps occur…

Calf muscle strains are painful and very tricky to recover from. Poor rehab often results in prolonged weakness and pain…

Painful Achilles tendon problems are common in people who perform repetitive running and jumping activities. It is also common in…

Do you have heel pain when first getting out of bed in the morning? You may be suffering from plantar…

Plantar fasciitis is one of the most commonly treated types of foot pain in physical therapy. Overuse or repetitive stress…

What are Ankle Sprains? Ankle sprains are one of the most common injuries that people experience. These injuries account for…