Chronic fatigue syndrome (CFS) results in persistent medically unexplained fatigue. For the diagnosis to be made symptoms are present for…

Many people visit a physical therapist after seeing a physician and being given a prescription to start physical therapy. However,…

Another new year is upon us and with it comes the resolution to get in shape, lose weight, or commit…

We are excited about our upcoming move to the Barnegat 67 Plaza. We expect to be open for business before…

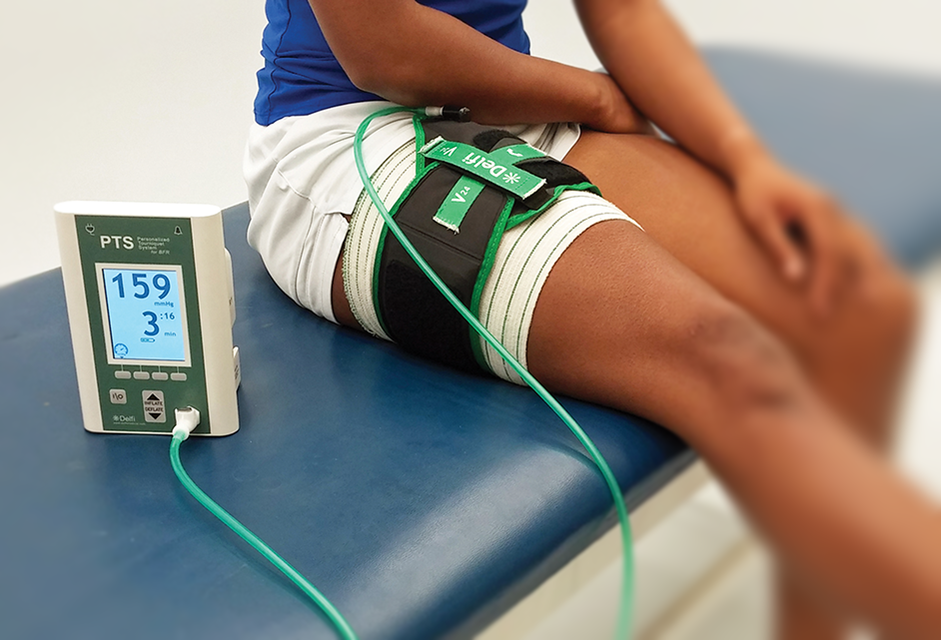
Blood flow restriction (BFR) therapy uses external pressure over a body part during exercise. The applied pressure allows the flow…
Many healthcare consumers are unaware of the fact that they are free to access the services of a physical therapist…

It’s not often that we are in agreement with insurance companies but they seem to be getting one thing right…
